Colonoscopy
- Home
- Colonoscopy

Colonoscopy
What is a Colonoscopy
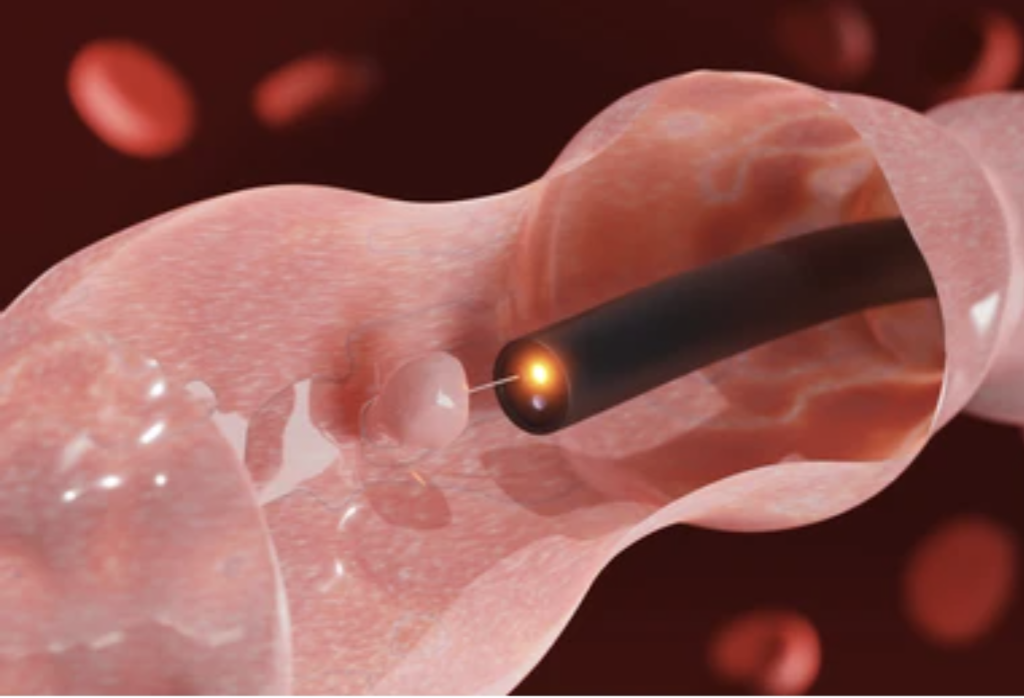
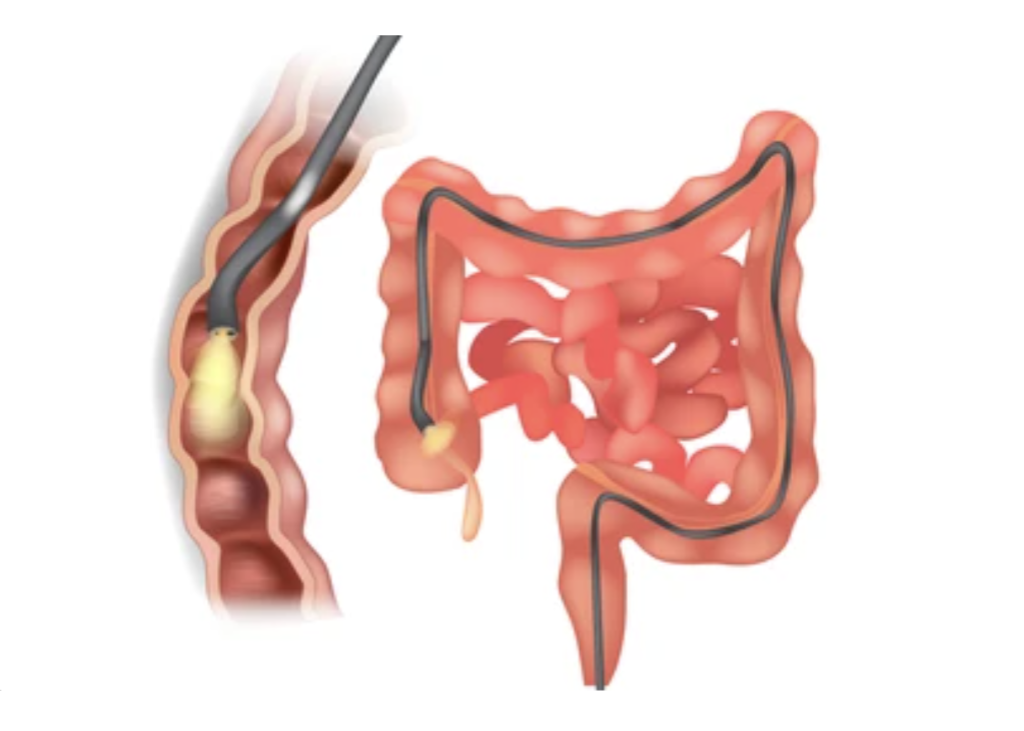
Colonoscopy is a safe, effective means of visually examining the lining of the bowel using a long, flexible, tubular instrument. It is used to diagnose and treat problems in the Ileum (lower or distal part of the small bowel), the colon including the rectum and anus. Colonoscopy allows Dr Merrett to take tissue samples (biopsies), to remove colon polyps and some superficial cancers and to perform dilatations of narrow segments that may be causing symptoms.
Most colonoscopies are done on an outpatient basis with minimal inconvenience and discomfort. It is performed by a gastroenterologist who is an accredited physician and is recognised by the Royal Australian College of Physicians as specialist in diagnosing and treating disorders of the bowel. Dr Merrett is certified by the Conjoint Committee.
What are the usual reasons for having a Colonoscopy?
Your referring doctor (usually your General Practitioner – GP) may recommend a colonoscopy exam if you have a change in bowel habits such as constipation or diarrhoea or bleeding, indicating a possible problem in the colon, rectum or anus.
Other reasons for Colonoscopy include
• Positive Faecal Occult Blood (FOB) test – these are sent out 2 yearly after the age of 50 years by the National Bowel Cancer Screening Program to all Australians
• Check unexplained abdominal symptoms
• Investigation of Iron Deficiency with or without anaemia
• Find and remove polyps or diagnose tumours seen on CT or PET scans
• Screen patients with a positive family history of bowel cancer
• Assess patients with Crohn’s disease / Ulcerative Colitis
• Monitor patients with a past history of colon polyps or cancer
How Is Colonoscopy Performed?
The bowel must first be thoroughly cleared of all faeces before a colonoscopy. This is done one to two days before the exam as prescribed by Dr Merrett. [See Colonoscopy Instructions].
On the day of colonoscopy you will be seen by a hospital nurse who will check all the admission details and check your pulse, blood pressure etc. The Anaesthetist will asses you to ensure you are fit and ready for the colonoscopy. The Anaesthetist will be by your side looking after you and administering appropriate medication to keep you comfortable and sleepy during the procedure. Finally, you will see Dr Merrett to discuss the preparation, asses any new symptoms and for any final questions.
The colonoscope is inserted through the anus and is then advanced to the portion of the colon where the small intestine enters into the large Intestine ie the caecum. Beyond the caecum is the Ileum. The lower or distal 20cm is usually examined. During a complete examination of the bowel, Dr Merrett will remove all polyps (where possible) or take biopsies as necessary.
The entire procedure usually takes less than 40 minutes. There is little pain because, sedation is given during the colonoscopy to relieve anxiety and discomfort. This will make you very sleepy. Following the colonoscopy, there may be slight discomfort and bloating although this is considerably less with experienced colonoscopists and with the use of CO2 insufflation. Most patients can resume their regular diet later that day. Because you are sedated during the colonoscopy you cannot drive and must make plans to be driven home by a relative/friend.
What Are The Benefits Of Colonoscopy?
With colonoscopy, it is now possible to detect and remove nearly all polyps and some superficial cancers without abdominal surgery. Colonoscopy is the most accurate method to detect colon polyps or early cancer. Frequently, polyps can be removed at the same time, a major step towards the prevention of colon cancer.
What Are The Risks Of Colonoscopy?
Most people experience no problems following a colonoscopy, however rare complications have occurred.
Gas Bloating – You may experience some abdominal cramping and excessive flatulence following a colonoscopy for a period of an hour or so. This problem is uncommon with experienced doctors and with the use of CO2 insfflation during the procedure.
Perforation – Rare. 1 in 5000 or less with experienced gastroenterologists. During the procedure the bowel wall tears and a hole is left in the bowel. A perforation is repaired by an operation that sometimes requires a temporary colostomy bag.
Bleeding – 1 in 500 times bleeding from the bowel can occur if a sample of bowel is taken or a polyp is removed. This is a problem that can be seen in patients taking blood thinning medications – Clopidogrel, Apixaban, Warfarin etc This may require a further colonoscopy to .fix or a blood transfusion or rarely surgery.
Aspiration – This can occur if you have not fasted properly before the colonoscopy there is a risk of inhaling stomach contents into the lung called aspiration. This can lead to pneumonia and occurs in about 1 in 1000 colonoscopies.
You must not drive a car for 24 hrs – if you do you will not be covered by insurance of any kind and have to pay the full costs of damages to any property or vehicle damaged in an accident whether you were at fault or not.
Failure – occasionally the colonoscopy may be incomplete. This is usually due to inadequate bowel preparation or to an excessively loopy bowel. If this occurs you may need to have the colonoscopy repeated after taking additional bowel preparation or you may need a CT scan. This is rarely required with experienced doctors.
Missed diagnosis – While colonoscopy is the best test for excluding bowel cancer it is not perfect and will not diagnose all cancers. There is a 4% chance that a colon cancer or polyp will be missed by this procedure. This can happen in the case of flat lesions that are particularly difficult to spot. The accuracy of Colonoscopy is increased with experienced Colonoscopists and by having a slow careful withdrawl of the colonoscope. The accuracy of Colonoscopy can be measured by the ADR – adenoma detection rate.
